Type 2 diabetes strikes people of all ages, and early symptoms are subtle. In fact, about one out of three people with type 2 diabetes don't know they have it. This chronic condition thwarts the body's ability to use the carbohydrates in food for energy. The result is elevated blood sugar. Over time, this excess sugar raises the risk for heart disease, loss of vision, nerve and organ damage, and other serious conditions.
Diabetes Warning Sign: Thirst
People with type 2 diabetes frequently have no symptoms. When symptoms do appear, one of the first may be an increase in thirst. This is often accompanied by additional problems, including dry mouth, increased appetite, frequent urination -- sometimes as often as every hour -- and unusual weight loss or gain.
Diabetes Warning Sign: Headaches
As blood sugar levels become more abnormal, additional symptoms may include headaches, blurred vision, and fatigue
Diabetes Warning Sign: Infections
In most cases, type 2 diabetes is not discovered until it takes a noticeable toll on health. One red flag is troubling infections, such as:
Cuts or sores that are slow to heal
Frequent yeast infections or urinary tract infections
Itchy skin, especially in the groin area
Diabetes Warning Sign: Sexual Dysfunction
Sexual dysfunction is common among people with diabetes. Diabetes can cause damage to blood vessels and nerve endings in the genitals, leading to a loss of feeling and making orgasm difficult. Other complications can include vaginal dryness and impotence in men. It's estimated between 35% and 70% of men with diabetes will have at least some degree of impotence in their lifetime. And about 1 in 3 women with diabetes will experience some form of sexual dysfunction.
Risk Factors You Can Control
Some health habits and medical conditions related to your lifestyle can increase the odds of developing type 2 diabetes, including:
Being overweight, especially at the waist
A sedentary lifestyle
Smoking
A diet high in red meat, processed meat, high-fat dairy products, and sweets
Abnormal cholesterol and blood fats, such as HDL "good" cholesterol lower than 35 mg/dL or a triglyceride level over 250 mg/dL
Risk Factors You Can't Control
Other risk factors are out of your control, including:
Race or ethnicity: Hispanics, African Americans, Native Americans, and Asians have a higher than average risk.
Family history of diabetes: Having a parent or sibling with diabetes boosts your risk.
Age: Being 45 and older increases your risk of type 2 diabetes.
The more risk factors you have, the greater your odds of developing type 2 diabetes.
Risk Factors for Women
Having gestational diabetes when you're pregnant puts you at higher risk for developing type 2 diabetes later on. Women who give birth to a baby weighing over 9 pounds are also at risk. Having a history of polycystic ovary syndrome can also cause insulin resistance that can lead to diabetes.
How Does Insulin Work?
In a healthy person, insulin helps turn food into energy -- in an efficient manner. The stomach breaks down carbohydrates from food into sugars, including glucose. Glucose then enters the bloodstream, which stimulates the pancreas to release insulin in just the right amount. Insulin, a hormone, allows glucose to enter cells throughout the body, where it is used as fuel. Excess glucose is stored in the liver.
Type 2 Diabetes: Metabolism Mishaps
In type 2 diabetes, the cells cannot absorb glucose properly. That means glucose levels in the blood become elevated. If you've developed a condition called insulin resistance, the body makes excess insulin, but the muscle, liver, and fat cells do not use or respond properly to the insulin. With long-standing uncontrolled type 2 diabetes, the pancreas will reduce the amount of insulin it produces.
Diagnosing Type 2 Diabetes
A simple blood test can diagnose diabetes. The A1C test gives a snapshot of your average blood glucose level over the past 2-3 months. An A1C level of 6.5% or higher may indicate diabetes. With a fasting plasma glucose test, a result above 126 is considered diabetes. Your doctor may order an oral glucose challenge test with a two-hour blood test. In people with classic symptoms of diabetes, a random blood glucose level of greater than 200 can help diagnosis diabetes.
Managing Diabetes: Diet
Fortunately, controlling blood sugar levels by changing diet can also cut your risk of complications. People with type 2 diabetes should carefully monitor carbohydrate consumption, as well as total fat and protein intake, and reduce calories. Ask your doctor for a referral to a registered dietitian to help you with healthy choices and an eating plan that will work for you.
Managing Diabetes: Exercise
Routine exercise, such as strength training or walking, improves the body's use of insulin and can lower blood sugar levels in people with type 2 diabetes. Being active also helps reduce body fat, lower blood pressure, and protect against heart disease. People with type 2 diabetes should try to get 30 minutes of moderate exercise on most days of the week.
Managing Diabetes: Stress Reduction
Stress can cause blood pressure to rise. It can also increase glucose levels in your blood as part of your "fight or flight" response. Or you may turn to food to cope with stress. All are bad when living with diabetes. Instead of letting stress take its toll, try practicing relaxation techniques such as deep breathing, meditation, or visualization. Sometimes talking to a friend, family member, counselor, or member of the clergy can help. If you're still battling stress, reach out to your doctor.
Managing Diabetes: Oral Medication
When people with type 2 diabetes are unable to control blood sugar sufficiently with diet and exercise, medication may be added. There are many types of diabetes pills available, and they are often used in combination. Some work by stimulating the pancreas to make more insulin, and others improve the effectiveness of insulin, or block the digestion of starches.
Managing Diabetes: Insulin
Your doctor may prescribe insulin early on in your treatment and in combination with pills. Insulin is also used in people with type 2 diabetes who develop "beta-cell failure." This means the cells in the pancreas no longer produce insulin in response to high blood sugar levels. In this case, insulin therapy -- injections or an insulin pump -- must become part of the daily routine.
Non-Insulin Injectables
New drugs are available for people with type 2 diabetes. Pramlintide (Symlin), exenatide (Byetta), and liraglutide (Victoza) are non-insulin injectable drugs. Whereas insulin pulls glucose into the cells, these medications cause the body to release insulin to control blood sugar levels.
Glucose Testing
Testing your blood glucose level will let you know how controlled your blood sugars are and if you need to take actions to change your treatment plan. How often and when you test will be based on how controlled your diabetes is, the type of therapy used to control your diabetes, and whether you are experiencing symptoms of fluctuating sugars. Talk with your doctor to find out how often you should use a glucose meter to check your blood sugar. Some common testing times may be when waking up, before and after meals and exercise, and at bedtime.
Continuous glucose monitor (GGM) may be useful to those with type 1 diabetes to help lower their blood glucose.
Long-Term Damage: Arteries
Over time, untreated type 2 diabetes can damage many of the body's systems. About two out of three people with diabetes die of heart disease. Having diabetes also puts you at a two to four times higher risk for stroke. People with diabetes are likely to develop plaque in their arteries, reducing blood flow and increasing risk of clots. This hardening of the arteries (atherosclerosis) raises the risk of heart attack and stroke.
Long-Term Damage: Kidneys
The longer you have diabetes, the greater the risk of developing chronic kidney disease. Diabetes is the leading cause of kidney failure, accounting for 44% of new cases in 2008. Controlling risk factors such as uncontrolled diabetes, high blood pressure, and high cholesterol reduces your risk of developing this complication. Annual screening for kidney disease and medications, which slow the development and progression of kidney disease, are used to reduce your risk of kidney failure.
Long-Term Damage: Eyes
High blood sugar can damage the tiny blood vessels that bring oxygen and nutrients to the retina, a critical part of the eye. This is known as diabetic retinopathy, and it can cause progressive, irreversible vision loss. It is the leading cause of new cases of blindness in people between the ages of 20 and 74. Pools of blood, or hemorrhages, on the retina of an eye are visible in this image.
Long-Term Damage: Nerve Pain
Over time, uncontrolled diabetes and elevated blood sugars create a very real risk for nerve damage. Symptoms can include tingling, numbness, pain, and a pins and needles sensation -- often in the fingers, hands, toes, or feet. The damage is not reversible, but treatments can help with the pain and numbness. And controlling your diabetes can help prevent further damage.
Long-Term Damage: Feet
Diabetic nerve damage can make it difficult to feel your feet and detect injury. At the same time, hardening of the arteries results in poor blood flow to the feet. Foot sores and gangrene can occur, even from small injury. In severe cases, infections can go unchecked and result in an amputation.
Preventing Type 2 Diabetes
One of the most astonishing things about type 2 diabetes is that such a life-altering condition is often preventable. To lower your risk, follow the same guidelines for warding off heart disease:
Eat a healthy diet.
Exercise for 30 minutes, five days a week.
Maintain a healthy weight.
Talk to your doctor about being screened for prediabetes.
In people with prediabetes, lifestyle changes and medication can help prevent the progression to type 2 diabetes.
please share if you think it is use ful for people who do not know their symptoms.
thanks deepak anand
my positive point for my life is.....To be hopeful in bad times is not just foolishly romantic. It

my positive point for my life is.....To be hopeful in bad times is not just foolishly romantic. It is based on the fact that human history is a history not only of cruelty, but also of compassion, sacrifice, courage, kindness. What we choose to emphasize in this complex history will determine our lives. If we see only the worst, it destroys our capacity to do something. If we remember those times and places -- and there are so many -- where people have behaved magnificently, this gives us the energy to act, and at least the possibility of sending this spinning top of a world in a different direction.
Thursday, March 29, 2012
Type 1 Diabetes and Pregnancy...........
Type 1 Diabetes and Pregnancy
Let your doctor know if you plan to become pregnant. When type 1 diabetes is poorly controlled, it can cause complications, including birth defects. Achieving good blood sugar control before conception lowers the risk of miscarriage and birth defects to a rate similar to that of the general population. It also reduces the risk of complications, such as dangerous increases in blood pressure and damage to the retina in the mother.
Type 1 Diabetes in Children
When a child is diagnosed with diabetes, it affects the whole family in a very practical way. Parents must help children monitor blood sugar, plan meals, and adjust insulin dosages around the clock. Because diabetes requires 24-hour maintenance, arrangements must be made for treatment during school and extracurricular activities. Laws vary from state to state regarding which employees may administer insulin at school.
Hope for an Artificial Pancreas
Researchers are developing a system dubbed the artificial pancreas -- a combination of an insulin pump and continuous glucose monitor controlled by a complex computer program. The goal is for the system to automatically release insulin in response to blood sugar levels, and to reduce the release of insulin when blood sugars drop, just the way a real pancreas does. Early trials suggest the approach can improve blood sugar control. An effective artificial pancreas could one day reduce the constant maintenance associated with type 1 diabetes.
Pancreatic Islet Cell Transplant
If insulin therapy fails to control your blood sugar or you have frequent insulin reactions, you may be a candidate for pancreatic islet cell transplant. Still an experimental procedure, a surgeon transfers healthy insulin-producing cells from a donor into the pancreas of someone with type 1 diabetes. Unfortunately, the results may last only few years. Medications used to prevent rejection are necessary and can have very serious side effects.
Type 1 Diabetes and Exercise
People with type 1 diabetes need to take precautions when exercising. To prevent a sudden drop in blood sugar, your health care team may recommend:
Checking your blood sugar before exercising
Adjusting your insulin dosage before exercising
Eating a snack before or during exercise
Your doctor may also suggest checking your urine for ketones, a sign that your blood sugar is too high. Avoid strenuous activity whenever ketones are present.
Type 1 Diabetes and Diet
There are many myths about what people with diabetes can and cannot eat. The reality is there are no "off limits" foods. You can eat sweets as part of a well-balanced diet and treatment plan. The key is to work with your health care team to balance your insulin therapy, meals, and level of physical activity.
Diabetes Treatment: Insulin Shots
Diabetes Treatment: Insulin Shots
Everyone with type 1 diabetes must take insulin to help the body process blood sugar. Most patients take insulin as an injection and need multiple shots per day. Your healthcare provider will explain how to adjust your insulin shots based on the results of your blood sugar testing. The goal is to keep glucose levels in the normal range as often as possible.
Insulin Reaction Warning Signs
Taking too much insulin can lower your blood sugar to dangerous levels. This is called an insulin reaction. These reactions can be mild, moderate, or severe, requiring the help of others. Warning signs include:
Exhaustion or excessive yawning
Being unable to speak or think clearly
Loss of muscle coordination
Sweating, twitching, turning pale
Seizures
Loss of consciousness
Neutralizing an Insulin Reaction
People who take insulin should carry at least 15 grams of a quick-acting carb at all times. Fast carbs are a way to bring the blood sugar up quickly to combat an insulin reaction. Examples include:
1/2 cup of fruit juice or non-diet soda
1 cup of milk
2 tablespoons of raisins
3 glucose tablets or 5 Lifesavers
If your blood sugar is still too low after 15 minutes, have another 15 grams. For a severe reaction, a drug called glucagon should be injected under the skin by a family member.
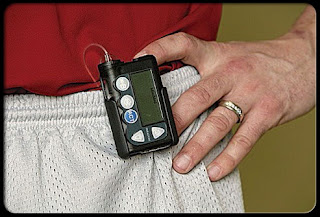
Diabetes Treatment: Insulin Pump
One way to reduce the odds of an insulin reaction is to use an insulin pump. This device provides insulin through a tiny tube inserted into the skin. It delivers insulin around the clock, eliminating the need for insulin shots. An insulin pump can help keep your blood sugar more stable and may allow more flexibility in planning your meals. Insulin pumps do have some disadvantages, so talk to your doctor to learn if this option is right for you.
How Well Is Your Treatment Working?
To find out how well your treatment is working, your doctor will probably suggest you have an A1c blood test every three to six months. This test reveals how well your blood sugar has been controlled over the past two to three months. If the results show poor blood sugar control, you may need to adjust your insulin therapy, meal planning, or physical activity.
How Well Is Your Treatment Working?
To find out how well your treatment is working, your doctor will probably suggest you have an A1c blood test every three to six months. This test reveals how well your blood sugar has been controlled over the past two to three months. If the results show poor blood sugar control, you may need to adjust your insulin therapy, meal planning, or physical activity.
Monitoring Your Blood Sugar
The first step toward preventing complications is to regularly monitor your blood sugar or glucose level. This involves pricking your finger, putting a drop of blood onto a test strip, and putting the strip into a glucose meter. The results will help you optimize your treatment plan. When your blood sugar stays near the normal range, you'll have more energy, fewer skin problems, and a reduced risk of heart disease and kidney damage.
In people with type 1 diabetes, the pancreas cannot make insulin. This vital hormone helps the body's cells convert sugar into energy. Without it, sugar builds up in the blood and can reach dangerous levels. To avoid life-threatening complications, people with type 1 diabetes must take some form of insulin for their entire lives.
Continuous Glucose Monitoring
Another way to check blood sugar patterns is with a continuous glucose monitoring system. A sensor measures the level of glucose in the tissue every 10 seconds and sends the information to a cell phone-sized device called a "monitor" that you wear. The system automatically records an average glucose value every five minutes for up to 72 hours. The device is not intended for day-to-day monitoring or long-term self-care, and it is not a replacement for standard blood sugar monitoring. It is only intended for use to discover trends in blood sugar levels.
What Is Type 1 Diabetes?
Warning Sign: Unusual Thirst
The symptoms of type 1 diabetes tend to come on suddenly and may include:
Feeling more thirsty than usual
Dry mouth
Fruity breath
Frequent urination
Many people with type 1 diabetes experience uncomfortable skin conditions, including:
Bacterial infections
Fungal infections
Itching, dry skin, poor circulation
Girls with type 1 diabetes are more likely to get genital yeast infections. Babies can develop candidiasis, a severe form of diaper rash caused by yeast that can easily spread from the
More Dangerous Signs
When blood sugars are not controlled, type 1 diabetes can cause more serious symptoms, such as:
Numbness or tingling in the feet
Blurred vision
Low blood sugar/hypoglycemia
Loss of consciousness
Some patients have no obvious warning signs before falling into a diabetic coma, which requires emergency treatment.
More Dangerous Signs: Ketoacidosis
Without treatment, type 1 diabetes deprives your cells of the sugar they need for energy. Your body starts burning fat for energy instead, which causes ketones to build up in the blood. These are acids that can poison the body. High levels of acid in your blood and the other abnormalities that result from the change in your blood's pH level may trigger a life-threatening coma known as diabetic ketoacidosis. This is an emergency that must be treated quickly and oftentimes in the hospital.
Type 1 vs. Type 2 Diabetes
In type 1 diabetes, the body's immune system mistakenly attacks and destroys the pancreatic cells that produce insulin. In type 2 diabetes, the pancreas is not under attack and usually produces enough insulin. But for numerous reasons, the body doesn't use the insulin effectively. The symptoms of the two forms are similar, but usually come on more rapidly in people with type 1.
Type 1 vs. Type 2 Diabetes
In type 1 diabetes, the body's immune system mistakenly attacks and destroys the pancreatic cells that produce insulin. In type 2 diabetes, the pancreas is not under attack and usually produces enough insulin. But for numerous reasons, the body doesn't use the insulin effectively. The symptoms of the two forms are similar, but usually come on more rapidly in people with type 1.
Type 1 vs. Type 2 Diabetes
In type 1 diabetes, the body's immune system mistakenly attacks and destroys the pancreatic cells that produce insulin. In type 2 diabetes, the pancreas is not under attack and usually produces enough insulin. But for numerous reasons, the body doesn't use the insulin effectively. The symptoms of the two forms are similar, but usually come on more rapidly in people with type 1.
Diagnosing Type 1 Diabetes
Simple blood tests can diagnose diabetes. A fasting blood sugar test or a random blood sugar test (plus the presence of symptoms) can be used. An A1c test, which reveals average blood sugar levels for the past 2-3 months, can also be used. Tests should be repeated on two separate days to diagnose diabetes. A less convenient glucose tolerance test will also help determine whether you have diabetes. If you're diagnosed with type 1 diabetes, your doctor may be able to determine the type by checking for certain antibodies in the blood.
Long-Term Complications
Prolonged high blood sugar can damage many of the body's systems over time. People with type 1 diabetes have a higher risk of:
Heart disease and stroke
Kidney failure
Vision problems and blindness
Gum disease and tooth loss
Nerve damage in the hands, feet, and organs
The symptoms of type 1 diabetes tend to come on suddenly and may include:
Feeling more thirsty than usual
Dry mouth
Fruity breath
Frequent urination
Warning Sign: Weight Loss
As blood sugar levels remain high, type 1 diabetes often leads to:
Unintentional weight loss
Increase in appetite
Lack of energy, drowsiness

Warning Sign: Skin ProblemsAs blood sugar levels remain high, type 1 diabetes often leads to:
Unintentional weight loss
Increase in appetite
Lack of energy, drowsiness

Many people with type 1 diabetes experience uncomfortable skin conditions, including:
Bacterial infections
Fungal infections
Itching, dry skin, poor circulation
Girls with type 1 diabetes are more likely to get genital yeast infections. Babies can develop candidiasis, a severe form of diaper rash caused by yeast that can easily spread from the
More Dangerous Signs
When blood sugars are not controlled, type 1 diabetes can cause more serious symptoms, such as:
Numbness or tingling in the feet
Blurred vision
Low blood sugar/hypoglycemia
Loss of consciousness
Some patients have no obvious warning signs before falling into a diabetic coma, which requires emergency treatment.
More Dangerous Signs: Ketoacidosis
Without treatment, type 1 diabetes deprives your cells of the sugar they need for energy. Your body starts burning fat for energy instead, which causes ketones to build up in the blood. These are acids that can poison the body. High levels of acid in your blood and the other abnormalities that result from the change in your blood's pH level may trigger a life-threatening coma known as diabetic ketoacidosis. This is an emergency that must be treated quickly and oftentimes in the hospital.
Type 1 vs. Type 2 Diabetes
In type 1 diabetes, the body's immune system mistakenly attacks and destroys the pancreatic cells that produce insulin. In type 2 diabetes, the pancreas is not under attack and usually produces enough insulin. But for numerous reasons, the body doesn't use the insulin effectively. The symptoms of the two forms are similar, but usually come on more rapidly in people with type 1.
Type 1 vs. Type 2 Diabetes
In type 1 diabetes, the body's immune system mistakenly attacks and destroys the pancreatic cells that produce insulin. In type 2 diabetes, the pancreas is not under attack and usually produces enough insulin. But for numerous reasons, the body doesn't use the insulin effectively. The symptoms of the two forms are similar, but usually come on more rapidly in people with type 1.
Type 1 vs. Type 2 Diabetes
In type 1 diabetes, the body's immune system mistakenly attacks and destroys the pancreatic cells that produce insulin. In type 2 diabetes, the pancreas is not under attack and usually produces enough insulin. But for numerous reasons, the body doesn't use the insulin effectively. The symptoms of the two forms are similar, but usually come on more rapidly in people with type 1.
Diagnosing Type 1 Diabetes
Simple blood tests can diagnose diabetes. A fasting blood sugar test or a random blood sugar test (plus the presence of symptoms) can be used. An A1c test, which reveals average blood sugar levels for the past 2-3 months, can also be used. Tests should be repeated on two separate days to diagnose diabetes. A less convenient glucose tolerance test will also help determine whether you have diabetes. If you're diagnosed with type 1 diabetes, your doctor may be able to determine the type by checking for certain antibodies in the blood.
Long-Term Complications
Prolonged high blood sugar can damage many of the body's systems over time. People with type 1 diabetes have a higher risk of:
Heart disease and stroke
Kidney failure
Vision problems and blindness
Gum disease and tooth loss
Nerve damage in the hands, feet, and organs
Subscribe to:
Posts (Atom)